Research by Dr. Cho Published in AACR's "Cancer Research"
By Camren Clouthier | April 19 2021A 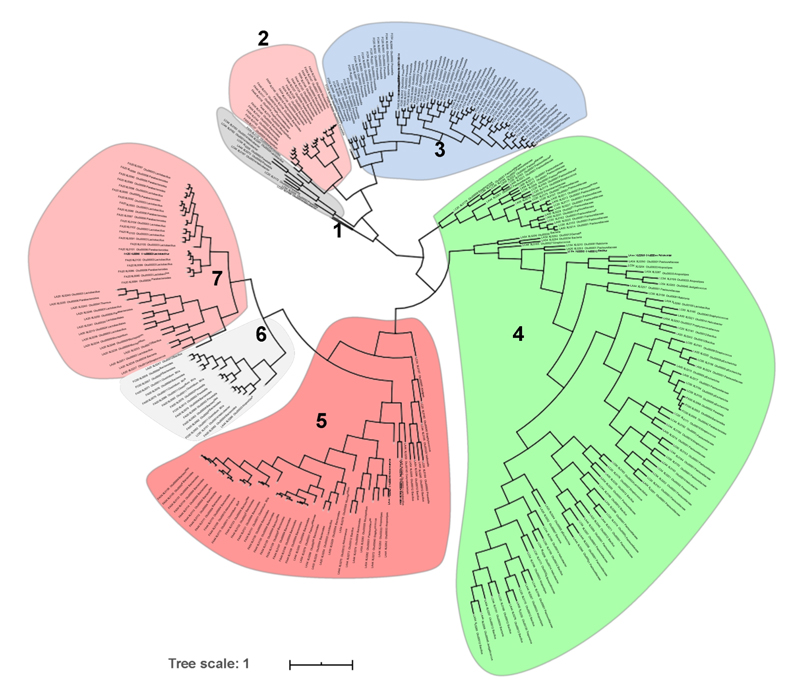 new publication from the Department of Pathology, led by Dr. Kathleen Cho, highlights how altering the microbiome within a mouse model of oviductal high-grade serious carcinoma can inhibit tumorigenesis. The study was just published in the American Association for Cancer Research's flagship journal. The research initiative also features contributions from faculty including Drs. Eric Fearon, Gabriel Nuñez and Naohiro Inohara.
new publication from the Department of Pathology, led by Dr. Kathleen Cho, highlights how altering the microbiome within a mouse model of oviductal high-grade serious carcinoma can inhibit tumorigenesis. The study was just published in the American Association for Cancer Research's flagship journal. The research initiative also features contributions from faculty including Drs. Eric Fearon, Gabriel Nuñez and Naohiro Inohara.
Past research has demonstrated that bacteria can influence the initiation and progression of cancers that arise in sites that harbor rich microbial communities, such as the colon. Little is known about the potential for the microbiome to influence tumorigenesis at sites considered sterile, including the upper female genital tract. However, the recent identification of distinct bacterial signatures associated with ovarian carcinomas suggests that microbiota in the gut, vagina, or elsewhere might contribute to ovarian cancer pathogenesis.
 Here, our team of experts tested whether altering the microbiome affects tumorigenesis in a mouse model of high-grade serous carcinoma (HGSC) based on conditional oviduct-specific inactivation of the Brca1, Trp53, Rb1, and Nf1 tumor suppressor genes. Cohorts of control (n=20) and antibiotic-treated (n=23) mice were treated with tamoxifen to induce tumor formation and then monitored for 12 months. The antibiotic cocktail was administered for the first 5 months of the monitoring period in the treatment group.
Here, our team of experts tested whether altering the microbiome affects tumorigenesis in a mouse model of high-grade serous carcinoma (HGSC) based on conditional oviduct-specific inactivation of the Brca1, Trp53, Rb1, and Nf1 tumor suppressor genes. Cohorts of control (n=20) and antibiotic-treated (n=23) mice were treated with tamoxifen to induce tumor formation and then monitored for 12 months. The antibiotic cocktail was administered for the first 5 months of the monitoring period in the treatment group.
Results showed that antibiotic-treated mice had significantly fewer and less advanced tumors than that of the control mice group at the endpoint. Furthermore, antibiotics induced changes in the composition of the intestinal and vaginal microbiota, which were present within the fecal samples. Clustering analysis showed that particular groups of microbiota are, in fact, associated with the development of HGSC in this model.
These findings demonstrate the microbiome influences HGSC pathogenesis in an in vivo model that closely recapitulates the human disease. Because the microbiome can modulate the efficacy of cancer chemo- and immunotherapy, the genetically engineered mouse model system may prove useful for testing whether altering the microbiota can improve the heretofore poor response of HGSC to immunotherapies.
—
The full publication within the American Association for Cancer Research is available here.
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
 ON THE COVER
ON THE COVER
