

"Leadership is not about titles, positions, or flowcharts. It is about one life influencing another,” John Maxwell.
In early 2020, the truth of this statement came to life in the Department of Pathology. Our country, our world, was faced with a pandemic caused by a novel virus for which no hard and fast answers were to be had. In the face of constantly changing “facts,” leadership in Pathology was found at all levels. It began with the Chair, Dr. Charles Parkos.
“As Chair, I feel privileged to lead a department where everybody pulled together as a team through a very physically and emotionally trying time. For me, I first became aware of SARS-CoV-2 over the winter of 2019-2020, right after the holidays. But the impact of this virus didn’t start sinking in until I was at the United States and Canadian Academy of Pathology (USCAP) Annual Meeting at the end of February/early March. Travel became restricted and the first cases were diagnosed in Washington State.” Parkos consulted with colleagues who were modeling the pandemic’s spread and quickly reached out to Dr. Riccardo Valdez, Director of Clinical Pathology, to ensure the department would be prepared for COVID.
"We were navigating circumstances that were unprecedented. We were going to have to do this together."
While Valdez initiated the test development process with the microbiology laboratory, Kristina Martin, Clinical Pathology Operations Director, immediately began working with the phlebotomy teams to make plans for protecting our staff in the blood draw stations. They drew up plans for how to isolate patients and what types of personal protective equipment (PPE) would be needed if they had symptomatic patients. “We thought we would have more time,” recalled Martin. “It escalated very quickly from there. I could never have imagined the impact it would have on our day-to-day lives.”
“I was in Los Angeles for the USCAP Annual Meeting, along with 5000 other pathologists, when we heard about this. None of us knew that it would be as serious as it was. Then we all came back to work and were facing a global public health crisis,” recounts Dr. Liron Pantanowitz, incoming Director of Anatomic Pathology. “I was just moving to Michigan at that time, so I had to move and assume a leadership position in a new institution during the pandemic.”
Dr. Jeffrey Myers, Vice Chair for Clinical Affairs and Director of Michigan Medicine Laboratories (MLabs), remembers hearing about Michigan’s first COVID case on National Public Radio on March 10th, then being at an all-day retreat on March 12th when he heard the announcement related to the campus shutdown. “I never imagined it would last as long as it did. In fact, I originally labeled my folder COVID: March – June; and that is kind of true, just not the same year. It became clear very, very quickly,” said Myers, “that there were a lot of questions. We were navigating circumstances that were unprecedented. We were going to have to do this together.”
On March 13, the COVID Preparedness and Response Team (CPRT) was formed in the Department of Pathology. This team was made up of leaders at all levels and across all missions of the department, both faculty and staff. Almost immediately, this team was challenged with staffing issues. All those whose work could be done remotely and those without patient care responsibilities were required to work offsite per the governor’s mandate. Those with patient care duties were put into two teams, Maize and Blue, in what was known as the Lombardy Schedule. This was to limit employee exposure to fewer individuals and to provide periods of respite through the pandemic. “The first communication from that group was on March 13,” stated Myers. “It was our work-from-home policies, which was the first thing to hit our radar screens. That and the use of PPE in our environments.” With faculty and staff working remotely and in shifts, communication was going to be key in weathering this pandemic. “There was a lot of anxiety and fear. This is completely understandable and valid,” Myers continued. “Around those anxieties and fears were opportunities for incomplete information or gaps in information that was exacerbating workplace stress. One of the things the CPRT team did was to create a slide deck to share information and encouraged faculty and staff to liberally share that deck with their own areas.” A regular email was also sent to all faculty and staff by Drs. Parkos, Myers, and Cho (Kathleen Cho, Vice Chair for Academic Affairs), to facilitate communications.
Nancy Fritzemeier, Anatomic Pathology Clerical Supervisor, was in the Lombardy region of Italy when the pandemic hit and came home just as things were ramping up. She recalled that the first thing she had to do was to split her administrative support staff into teams, ensuring that all work areas were covered and the workload was balanced so that the clinical work could still get done. “My staff were great. There was never an issue and people just said OK. There was no pushback at all.” This process was repeated across all areas of the department with similar results. With so many people working remotely, many faculty and staff volunteered to provide services in areas that needed assistance. “I was really amazed at how many of our faculty and staff stepped up to the plate to help with patient management,” said Parkos.
"I was really amazed at how many of our faculty and staff stepped up to the plate to help with patient management."
 “My first concern was the safety of the employees and how we were going to support the labs and what they would need through the pandemic,” explained Regina Ferguson, Pathology Facilities Manager for Clinical and Research Pathology. The logistics required to implement the necessary measures were mind-boggling and included everything from telecommunications for those working remotely, to the demand for laboratory equipment, to the need for medical supplies, which far exceeded the actual supply. The need for additional freezers to hold testing reagents is one example. Everyone was buying freezers, and they were becoming difficult to find. Even when purchased, it wasn’t as simple as just plugging it in. There needed to be sufficient power, proper ventilation, adequate backup power, storage space, and connected monitoring. Building access modifications were another ongoing challenge. Per the Governor’s guidelines, building access was restricted, making it challenging for research personnel to obtain building access. Work schedules had to be adjusted to maintain their critical research. Construction projects and scheduled installations were placed on temporary hold. Deliveries needed to be coordinated so access could be granted. It was a team effort with facilities, construction services, maintenance, procurement, and IT.
“My first concern was the safety of the employees and how we were going to support the labs and what they would need through the pandemic,” explained Regina Ferguson, Pathology Facilities Manager for Clinical and Research Pathology. The logistics required to implement the necessary measures were mind-boggling and included everything from telecommunications for those working remotely, to the demand for laboratory equipment, to the need for medical supplies, which far exceeded the actual supply. The need for additional freezers to hold testing reagents is one example. Everyone was buying freezers, and they were becoming difficult to find. Even when purchased, it wasn’t as simple as just plugging it in. There needed to be sufficient power, proper ventilation, adequate backup power, storage space, and connected monitoring. Building access modifications were another ongoing challenge. Per the Governor’s guidelines, building access was restricted, making it challenging for research personnel to obtain building access. Work schedules had to be adjusted to maintain their critical research. Construction projects and scheduled installations were placed on temporary hold. Deliveries needed to be coordinated so access could be granted. It was a team effort with facilities, construction services, maintenance, procurement, and IT.
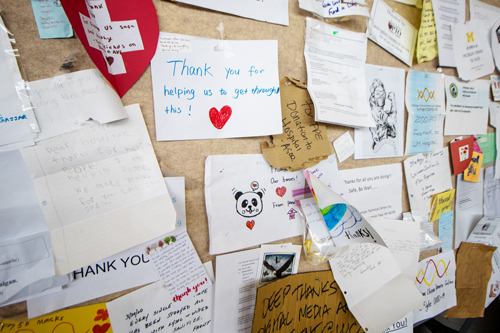 Within the department, there were multiple safety measures instituted to keep staff safe. Christine Rigney, Director of Operations for the Division of Anatomic Pathology, and Jennifer Bell, Safety and Preparedness Coordinator, were assigned responsibility for many of these measures. “There was a lot of information coming out quickly and changing quickly,” said Rigney. “It was very confusing and upsetting to many. We strove to communicate in as many ways as possible and with sufficient frequency to be sure everyone knew what to do.” Rigney, Bell, and Ferguson worked hand-in-hand with engineering to introduce on-site safety protocols including installation of plexiglass dividers between work stations, around multi-headed microscopes, patient waiting areas, and other areas where 6-foot social distancing was not feasible. Seating was removed in conference rooms to prevent overuse. Posters on walls and elevators with stickers on floors reminded faculty and staff to maintain social distancing. Early in the pandemic, there was a severe mask shortage, which required staff to reuse single-use masks. Plus, hand sanitizer was difficult to obtain. “There were huge challenges to maintain our own safety and health. The way we overcame any of the challenges was as a team,” said Rigney. “I think one of the things that left a super awesome impression on me was the way the entire medical system pulled together to work in lock-step, focusing on the one mission of taking care of the patients and taking care of our staff. When we all had the same major priority, I could see how powerful we really were and how great Michigan Medicine really is. While it was scary, it made me feel extra proud of who I work for.”
Within the department, there were multiple safety measures instituted to keep staff safe. Christine Rigney, Director of Operations for the Division of Anatomic Pathology, and Jennifer Bell, Safety and Preparedness Coordinator, were assigned responsibility for many of these measures. “There was a lot of information coming out quickly and changing quickly,” said Rigney. “It was very confusing and upsetting to many. We strove to communicate in as many ways as possible and with sufficient frequency to be sure everyone knew what to do.” Rigney, Bell, and Ferguson worked hand-in-hand with engineering to introduce on-site safety protocols including installation of plexiglass dividers between work stations, around multi-headed microscopes, patient waiting areas, and other areas where 6-foot social distancing was not feasible. Seating was removed in conference rooms to prevent overuse. Posters on walls and elevators with stickers on floors reminded faculty and staff to maintain social distancing. Early in the pandemic, there was a severe mask shortage, which required staff to reuse single-use masks. Plus, hand sanitizer was difficult to obtain. “There were huge challenges to maintain our own safety and health. The way we overcame any of the challenges was as a team,” said Rigney. “I think one of the things that left a super awesome impression on me was the way the entire medical system pulled together to work in lock-step, focusing on the one mission of taking care of the patients and taking care of our staff. When we all had the same major priority, I could see how powerful we really were and how great Michigan Medicine really is. While it was scary, it made me feel extra proud of who I work for.”
The Pathology Informatics (PI) Team was instrumental in ensuring the department continued to function throughout the pandemic. When the work-at-home order was issued, the PI team was tasked with ensuring faculty, staff, and trainees possessed the hardware and software necessary to connect from home. Laptops, docking stations, monitors, printers, and other equipment needed to be procured, set up, and deployed virtually overnight. They were also responsible for ensuring proper connectivity of label printers and interfaces for test ordering in the new, temporary COVID locations for the Emergency Department, at Mott Children’s Hospital and Von Voigtlander Women’s Hospital, in the Respiratory Infection Containment Unit, at the testing tents, and for the planned field hospital, which was thankfully, not needed. Zoom became the communication method of choice and PI desktop support spent hours on the phone with new Zoom users helping them learn how to use this tool effectively. In addition, data were needed by the leadership team, so PI teamed up with the Division of Quality and Health Improvement to create a COVID dashboard. This dashboard enabled managers to monitor workloads, adjust staffing, and procure supplies in a timely manner. “Communication was the key to success,” said Ferguson. “Each morning at 7 am, I meet with Peggy Otto (Administration), Oliver Bichakjian (PI), Steve Marshall (PI), and Eileen McMyler (PI) by Zoom to talk about upcoming projects and to make sure everyone is on the same page.”

Pathology was committed to caring for its employees through the pandemic and beyond. Difficult family situations or COVID fatigue caused some to be unable to perform their standard work responsibilities for a time. “We redeployed staff to keep people working and to balance workloads. We kept staff employed who had childcare or other issues,” said Rigney. “If they could work from home, we had them working on our Quality Assurance documentation, CAP checklists, or writing procedures that needed to get completed. We had to be really creative to keep people working whether they were at work or at home, to fit their circumstances. We didn’t want them to feel like they didn’t have many options.”
“I truly appreciate the sacrifices made by our faculty and staff. We have all been changed by this pandemic and our workplace will be forever changed. I am optimistic that it will be a better place because we have found ways that we can do things better and keep people happier,” said Parkos. Fritzemeier added, “We had strong leadership that made people feel safe. We had clear direction on how we were going to deal with the pandemic at the departmental level. The sense of community really stepped up and people were helping each other without any fussing or judgments. We were a team.” People learned to be gracious and kind to one another. Pantanowitz concluded, “We have to be kind. This was not the time to be harsh. We need to really understand and listen to people. To have kind policies, to let people work from home. With that recipe, we will be successful – and we have been successful.”